The Bidirectional Relationship Between Fatty Liver and High Blood Pressure
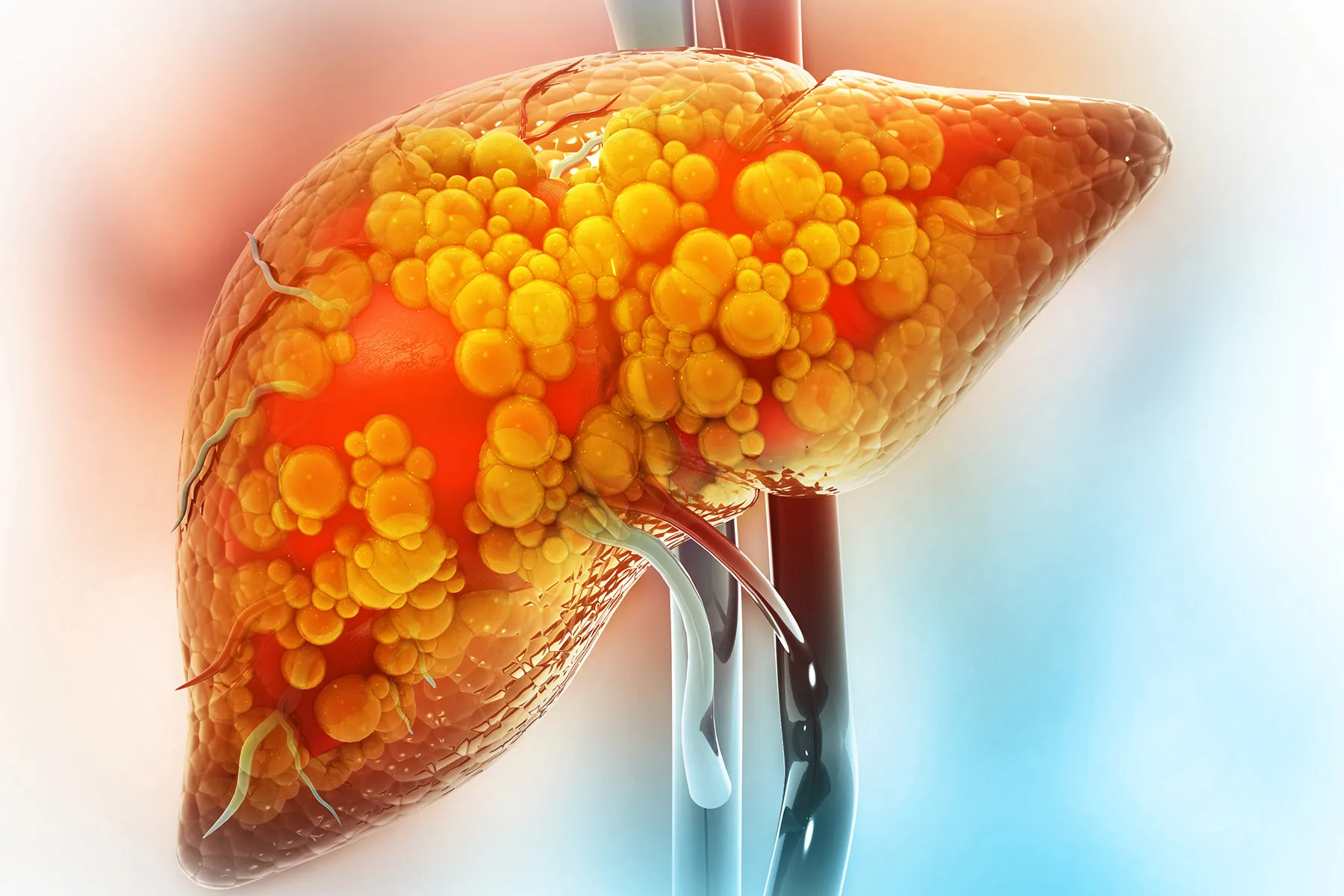
Metabolic dysfunction-associated steatotic liver disease (MASLD, formerly known as non-alcoholic fatty liver disease, NAFLD) and high blood pressure are closely linked. Approximately 40% of MASLD patients also have high blood pressure, while 50% of hypertensive patients exhibit fatty liver. This bidirectional relationship may be driven by the following mechanisms:
- Systemic Inflammation
Fatty liver can trigger chronic inflammation, activating the sympathetic nervous system and leading to vasoconstriction and elevated blood pressure. Research from Hong Kong University highlights that excessive secretion of FGF21 in fatty liver may exacerbate systemic inflammation, further impacting blood pressure regulation:cite[1]. - Insulin Resistance
Insulin resistance is a common pathological basis for both conditions. Fat accumulation in the liver worsens insulin signaling abnormalities, while hyperinsulinemia promotes sodium retention in the kidneys, increasing blood volume and pressure:cite[6]. - Oxidative Stress and Vascular Dysfunction
Fatty liver leads to an accumulation of free radicals, damaging vascular endothelial function and inhibiting nitric oxide-mediated vasodilation, ultimately causing vasoconstriction and hypertension. Oxidative stress plays a significant role in this process:cite[2].
Overlapping Risk Factors
Obesity, diabetes, and high cholesterol are shared risk factors for both fatty liver and high blood pressure. Studies show:
- Obesity: 50%-90% of obese individuals have fatty liver;
- Co-occurrence: Patients with both conditions face a 2-3 times higher risk of atherosclerosis compared to those with only one condition;
- Uncontrolled Hypertension: Blood pressure levels above 130/80 mmHg accelerate liver fibrosis and significantly increase all-cause mortality:cite[6]:cite[7].
Integrated Management Strategies
Lifestyle Interventions
- Dietary Adjustments: Adopt a Mediterranean diet, limit red meat and refined sugars, and increase fiber and omega-3 fatty acid intake (e.g., from fatty fish);
- Weight Management: A 5%-10% reduction in body weight can significantly improve liver fat content and blood pressure levels;
- Regular Exercise: Engage in at least 150 minutes of moderate-intensity aerobic exercise weekly (e.g., brisk walking, swimming) to reduce liver fat and enhance vascular elasticity.
Medications and Monitoring
- Antihypertensive Drugs: Angiotensin receptor blockers (e.g., losartan) may also improve liver fibrosis;
- Metabolic Control: Use statins to manage high cholesterol and maintain HbA1c levels below 7%;
- Liver Health Assessment: High-risk individuals should regularly monitor ALT, AST, and liver stiffness via FibroScan:cite[4]:cite[6].
:max_bytes(150000):strip_icc()/GettyImages-1390886687-a344488657004e5d86a55071aa486aec.jpg)
Consequences of Untreated Conditions
- Liver Complications
Fatty liver can progress to cirrhosis and even liver cancer. Studies indicate that MASLD patients with hypertension experience a 30% faster progression of liver fibrosis:cite[1]. - Cardiovascular Events
The synergy between the two conditions significantly increases the risk of myocardial infarction and stroke. Research from Leiden University Medical Center using cardiac MRI found that a 5% increase in liver fat correlates with an 8% decline in left ventricular diastolic function:cite[6]. - Systemic Metabolic Disorders
Long-term untreated conditions can exacerbate type 2 diabetes, chronic kidney disease, and cognitive decline:cite[7].
Frequently Asked Questions
Q: Does fatty liver directly cause high blood pressure?
The causal relationship remains unclear, but both conditions exacerbate each other through mechanisms like inflammation and oxidative stress.
Q: Which antihypertensive drugs benefit the liver?
Losartan and other ARBs may reduce liver fat deposition, though more clinical validation is needed:cite[6].
Q: How does cirrhosis affect blood pressure?
Advanced cirrhosis can lead to portal hypertension, a specific type of high blood pressure requiring targeted treatment to reduce portal vein pressure:cite[6].